Attempting to understand viruses and how they cause disease *may also contain other biological material
Sunday, 21 November 2010
Epithelial defence – the role of highly reactive oxygen species
Friday, 19 November 2010
Stopping pathogens at the portal of entry: mucous membrane defence

Fig 1. Mucosal epithelium found within the respiratory tract http://farm4.static.flickr.com/3346/3661529896_fd19543c7f.jpg
Azizi A, Kumar A, Diaz-Mitoma F, Mestecky J (2010)
The immune system in the gastrointestinal tract plays a crucial role in the control of infection, as it constitutes the first line of defense against mucosal pathogens. The attractive features of oral immunization have led to the exploration of a variety of oral delivery systems. However, none of these oral delivery systems have been applied to existing commercial vaccines. To overcome this, a new generation of oral vaccine delivery systems that target antigens to gut-associated lymphoid tissue is required. One promising approach is to exploit the potential of microfold (M) cells by mimicking the entry of pathogens into these cells. Targeting specific receptors on the apical surface of M cells might enhance the entry of antigens, initiating the immune response and consequently leading to protection against mucosal pathogens. In this article, we briefly review the challenges associated with current oral vaccine delivery systems and discuss strategies that might potentially target mouse and human intestinal M cells.
Different parts of our bodies are not equally vulnerable to infection and we can consider our immune system to be differentially active across all anatomical sites. One of the biggest sites of pathogen entry is the mucosal epithelium which lines our internal parts including the respiratory, gastrointestinal and urogenital tracts (fig 1.).
These surfaces have been estimated to cover 200x the area that our skin covers and if you think about it, most pathogens will use one of these openings to the outside world to gain entry into our bodies: measles virus via the respiratory tract; HIV through the urogenital tract; and E.coli from the gastrointestinal tract. It is this reason that we expend so much energy and effort in keeping these areas protected from would-be dangerous micro-organisms.
Fig. 2. Dipiction of the mucosal immune system:inductive and effector sites both present with mechanisms of inductive and nuetralisation (SIgA) shown. Notice the MALT complex (M cells, antigen presenting cells and B/T cells). http://www.nature.com/mi/journal/v1/n1/fig_tab/mi20079f1.html
Mucosal immunity is a complex system of anatomical, cellular and molecular 'innate' components: epithelial cells which line the mucosa form very tight layers which prevent bacteria or viruses from penetrating deeper into the body; these cells also secrete a number of antimicrobial compounds and enzymes and can rapidly respond to infection through protein mediated cell-cell signalling establishing intra-cellular protection.
In order to mount an efficient response there is a close association between the mucosal epithelium and lymphoid tissues. This 'mucosa-associated lymphoid tissue' or MALT (examples including nasal-associated lymphoid tissue or NALT and gut-associated ymphoid tissue or GALT) is formed by a close interaction between the epithelial lining (antigen sampling 'M' cells) and underlying immune cell complexes consisting of antigen-presenting cells, T cells and B cells.
These mucosal sites – interestingly – form a collective adaptive unit across the whole body when we consider anti-microbial immunity. This 'common mucosal immune system' is mediated by a network of inductive and effecter sites located within the MALT: inductive sites sensing pathogen activity at one area can generate cellular immune responses which can travel systemically from one site to another (e.g. NALT to GALT) . One of the major players in this immunity is a special type of antibody known as secretory immunoglobulin A (SIgA) which is transported from the underlying immune tissue at effector sites to the surface of the mucosa above and can interact with and bind to pathogens and prevent infection and/or damage being done (see fig2 and fig3).
Interest has stemmed from the thought that if we were able to generate adequate antibody responses at the pathogen site of entry (SIgA at the mucosa) we may able to prevent infection from occurring before it is too late and infection has spread from primary areas to other tissues causing significant disease . Current vaccination strategies have focussed on the development of systemic IgG antibodies without consideration for those found at initial portals of entry and although many have been successful for some diseases, the millions of deaths stemming from pathogen-mucosa related infections warrant further investigation and targeting. The question is which inductive MALT site is best suited for vaccination which in turn depends upon pathogen entry strategy, ease of administration, particular side effects and the relative ability of particular MALTs to develop effecter functions at different mucosal epithelium. To date the most promising of strategies lies with nasal or oral vaccine delivery systems and much research has been carried out in order to improve the efficacy of each.
Fig 3. Cartoon dipicting the general structure of the five basic antibodies in humans: IgA the one concerned with mucosal immunity. http://www.cartage.org.lb/en/themes/sciences/lifescience/generalbiology/physiology/LymphaticSystem/Antibodymediated/AntiBtypes.gif
Novel approaches have been used to target vaccines to those cells responsible for antigenic sampling found across most mucosal surfaces – the M cells. These cells can transport antigenic materials from the epithelial lining to the underlying lymphoid complexes via antigen-presenting cells. These cells however are present in low numbers (1 in 10 million epithelial cells are M cells in the GI tract) with the mucosa hence specific targeting may facilitate higher antigen uptake and greater immune induction and these strategies can be adapted to both respiratory and oral delivery systems depending on the vaccine.
We are only now beginning to see the outcome of current research into mucosal immunity and vaccines. Disrupting the close relationship between pathogens and the mucosa is paramount in preventing the millions of deaths worldwide from mucosal-borne infections and the concurrent development of novel targeting and vaccination strategies we may well witness the generation of highly effective, easily administered and most importantly safe vaccines for the most dangerous known diseases: AIDS; cholera; and influenza.
Azizi A, Kumar A, Diaz-Mitoma F, Mestecky J (2010) Enhancing Oral Vaccine Potency by Targeting Intestinal M Cells. PLoS Pathog 6(11): e1001147. doi:10.1371/journal.ppat.100114
Friday, 29 October 2010
Viral genomes in High Definition
As seen with cellular organisms, our ability to rapidly and accurately sequence multiple viral genomes at low cost is being overtaken by our inability to analyse the functional roles that certain genes – including regions within genes- play in a range of phenotypic processes during an infection. Lack of functional studies represents a major roadblock to understanding the basic biology of these pathogenic organisms and prevents us from generating safe and efficacious vaccines or virotherapies.
High-Resolution Functional Mapping of the Venezuelan Equine Encephalitis Virus Genome by Insertional Mutagenesis and Massively Parallel Sequencing
Brett F. Beitzel, Russell R. Bakken, Jeffrey M. Smith, Connie S. Schmaljohn*
The United States Army Medical Research Institute of Infectious Diseases, Fort Detrick, Maryland, United States of America
We have developed a high-resolution genomic mapping technique that combines transposon-mediated insertional mutagenesis with either capillary electrophoresis or massively parallel sequencing to identify functionally important regions of the Venezuelan equine encephalitis virus (VEEV) genome. We initially used a capillary electrophoresis method to gain insight into the role of the VEEV nonstructural protein 3 (nsP3) in viral replication. We identified several regions in nsP3 that are intolerant to small (15 bp) insertions, and thus are presumably functionally important. We also identified nine separate regions in nsP3 that will tolerate small insertions at low temperatures (30°C), but not at higher temperatures (37°C, and 40°C). Because we found this method to be extremely effective at identifying temperature sensitive (ts) mutations, but limited by capillary electrophoresis capacity, we replaced the capillary electrophoresis with massively parallel sequencing and used the improved method to generate a functional map of the entire VEEV genome. We identified several hundred potential ts mutations throughout the genome and we validated several of the mutations in nsP2, nsP3, E3, E2, E1 and capsid using single-cycle growth curve experiments with virus generated through reverse genetics. We further demonstrated that two of the nsP3 ts mutants were attenuated for virulence in mice but could elicit protective immunity against challenge with wild-type VEEV. The recombinant ts mutants will be valuable tools for further studies of VEEV replication and virulence. Moreover, the method that we developed is applicable for generating such tools for any virus with a robust reverse genetics system.
Beitzel et al recently publish the development of a ‘high-resolution genomic mapping technique’ that will facilitate the easier investigation of particular viral genes in a range of virus/host interactions. Venezuelan equine encephalitis virus, endemic to South America, is an important zoonotic pathogen that continually re-emerges from its rodent reservoir via a mosquito vector causing potentially fatal encephalitis in both humans and horses. There is currently no vaccines or anti-viral treatments for this disease and the exact roles that each of its 8 proteins play in its basic biology and replication are currently being investigated, hoping to yield helpful insight.
Studying the role of nsP3 gene in VEEV but later expanding it the rest of the genome, the group used a technique called transposon mutagenesis in which a short (15 nucleotides) DNA fragment is inserted randomly into the target gene or genome being studied. They generated a large cDNA library with high coverage in that every nucleotide had been targeted around 200 times and using high- throughput DNA sequencing were able to map the inserts at a high resolution and record the frequency that they were present at. Combining this with a reverse genetics system, they generated recombinant infectious virus carrying and expressing the inserts in order to assess their function in replication and initially, the group assessed the role that these inserts had on replication at particular temperatures.
By altering the temperatures in which the viruses were grown they were to able to effectively screen for a particular phenotype (the ability to grow at 40 degrees for example) and easily map the locations that would and would-not tolerate the 15bp insertions. Using this method they generated temperature sensitive (ts) mutants that were able to replicate at one temperature (30) and not at another (40).
Monday, 18 October 2010
Viral control with endosymbiotic bacteria - the dengue story
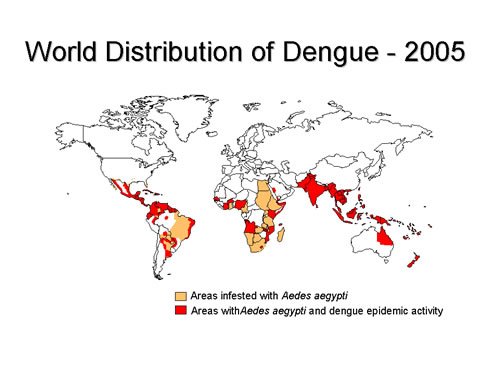
Fig.1. WHO stats on DENV distribution 2005
Dengue viruses cause what is known as a severe “flu-like” illness including symptoms such as rash, mild/high fever, headache and muscle pain. Although it is rarely fatal, in some instances it can develop into Dengue Haemorrhagic Fever (DHF), a potentially deadly complication. There are generally considered four sub-types (DENV-1 to 4) of Dengue virus due to the sufficient antigenic differences exhibited between them leading to little or no effective cross-neutralisation making it difficult to develop a ‘universal’ Dengue vaccine or treatment. The viruses are spread by certain Aedes species of mosquito passing infectious virus on during feeding by the females and due to the lack of treatments, the inhibition of mosquito activity has been seen as key to Dengue prevention.
A number of ‘vector control’ methods are being carried out to limit mosquito-human viral transmission which focus on disrupting the ecological niche in which the vector requires to breed – in this case stagnant water pools found in urban areas in which larva are found (e.g. rainwater filled tyres and cups). One major strategy is the biological control of Aedes populations including the use of mosquito larvae preying fish and invertebrates, release of Aedes infecting viruses or by genetic modification of mosquito genomes. An attractive means of control has come from the realisation that certain bacterial species (Wolbachia) - and only a specific strain of it - which naturally infects mosquitoes and other insects could inhibit dengue virus transmission thus negating the need for transgenic mosquitoes in the environment. These obligate, intracellular parasites which survive in the host cell’s cytoplasm are passed maternally from generation to generation. The bacteria can affect the mosquitoes and dengue virus in a number of ways, both general and specific for example: reduced lifespan of Aedes hosts; reduced dengue virus replication; increased antiviral immunity; and spatial exclusion of virus from the cytoplasm.
Fig.2. DENV transmission in Aedes species http://activity.ntsec.gov.tw/lifeworld/english/content/images/en_dis_c10.jpg
Frentiu et al report their investigations into the mechanism of reduced viral (dengue virus serogroup 2) replication at the cellular level paralleling earlier observations of whole organism Wolbachia infection. Their transition to a cell-culture experimental system may facilitate easier study of viral-host interactions and the group documents significantly reduced dengue virus replication in Wolbachia infected cell lines compared to non-infected controls possibly being related to an increased bacterial density within the cytoplasm. A bacterial ‘priming’ of the insect immune system may also contribute to decreased replication. They also show evidence that Wolbachia infected mosquitoes may display a fitness benefit compared to those not infected when challenged with dengue virus. This predicted increased fitness in the wild may aid the use of this biological control technique in a natural ecosystem. Measures such as these will benefit from the large, field trials already planned to study Aedes-Wolbachia interactions.
Fig.3. Wolbachia (Green) within a drosophila embryo imaged by confocal microscopy. http://www.genetics.org/content/vol178/issue4/cover.dtl
 Dengue virus is an important emerging arthropod-borne pathogen worldwide and is predicted to further increase its range into more temperate regions. Currently there is no effective vaccine or treatment and much research has focused on the interactions between virus and Aedes mosquito including the use of intracellular bacterial pathogens to limit viral replication and transmission. A number of strategies have been studied and seem attractive on a wider scale in endemic countries however the mechanisms of DENV/Wolbachia interactions and the effects on arthropods in the wild are understudied. Frentiu et al highlight the importance of a mechanistic understanding of dengue control and the development of novel control strategies.
Dengue virus is an important emerging arthropod-borne pathogen worldwide and is predicted to further increase its range into more temperate regions. Currently there is no effective vaccine or treatment and much research has focused on the interactions between virus and Aedes mosquito including the use of intracellular bacterial pathogens to limit viral replication and transmission. A number of strategies have been studied and seem attractive on a wider scale in endemic countries however the mechanisms of DENV/Wolbachia interactions and the effects on arthropods in the wild are understudied. Frentiu et al highlight the importance of a mechanistic understanding of dengue control and the development of novel control strategies.



