Fig.1 NiV infection in an epithelial cell monolayer and different time points and stained (red). Epithelial adhesion indicated in green.
Nipah virus (NiV), an emerging and deadly paramyxovirus of bat origin has been responsible for a number of fatal outbreaks of disease in humans and other animals in South-East Asia and as of yet no vaccine or therapy exists. The mucosal epithelium of the host respiratory tract is believed to be the most common route of viral spread in humans and from this primary site the virus can disseminate systemically through the blood system resulting in rapid endothelial dysfunction and vasculitis. Viruses must overcome a number of cellular mechanical barriers in order to establish efficient infection and knowledge of how they do this is key to understanding pathogenesis and infection in general.
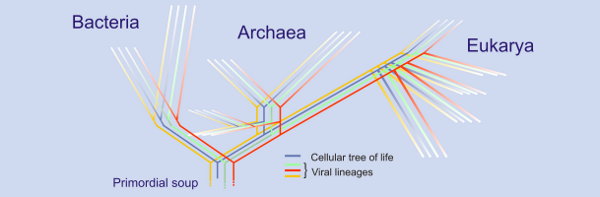
The ability to move between and within cells is central to viral transmission and pathogenesis. Viruses - as obligate intracellular parasites – need to effectively enter and exit target cells within the host organism in which they reside and establish productive infections to facilitate transmission and replication. Viruses generally use two methods of spreading – cell free and cell associated transmission; the first requiring assembly and budding of mature virus from the cell membranes and the second taking advantage of the close association between host cells, facilitating the union of the membranes of two separate cells. The relative roles of each of these processes in vivo and in transmission and infection are not fully known.
The NiV F and G glycoproteins are responsible for virion-host cell membrane fusion and also cell-cell fusion via interactions with NiV receptors expressed in the plasma membrane of target cells. The mechanism of viral spread within the host are thus very important in elucidating how the virus causes disease and transmits itself within a population; polarised epithelial surfaces – where the apical and basolateral domains are structurally and functionally distinct–playing dual roles in initial entry and host-host viral spread.
Fig.2. NiV virion - notice the fusion and attachement proteins on the surface (red and green). http://www.bepast.org/docs/photos/Nipah%20Virus/nipah%20virus.jpg.

Viruses have taken advantage of the fact that host cells require discrete functions on their apical and basolateral domains and can preferentially target mature virus formation to particular cellular locations through intrinsic protein signals built in to their glycoproteins. Apical release will generally facilitate free virion spread and host-host transmission (e.g in the respiratory tract) while basolateral release may allow direct cell-cell spread and could lead to systemic infections not restricted to the particular primary site of replication. NiV can therefore control its transmission within and between hosts by targeting its infection machinery (F and G glycoproteins) to either the apical or basolateral surfaces of polarised cells.
Fig.3. Polarised epithelial cell monolayer. Apical and basal domains shown. http://www-dsv.cea.fr/var/plain/storage/original/media/File/IBITECS/SB2SM/Eq%20Verbavarz/Cell-base.JPG

A recent paper has investigated the mechanism of NiV spread in polarised epithelium in vitro using cell imaging and molecular analyses of its F and G glycoproteins. They demonstrate that the NiV glycoproteins can facilitate cell-cell spread within polarised epithelial cells through targeting to basolateral cell surfaces between closely positioned cells allowing entry to epithelial cells or underlying tissues. They also note that they are also found on the apical domain allowing efficient spread via free virus release. The group explored the functional importance of such targeting by determining the exact molecular signals required for such protein trafficking and then disrupting them. By purposely retargeting the fusion machinery to the apical side, NiV cell-cell spread by lost. The group also report their findings of NiV infection within infected endothelial cells – a major target of NiV – and establish that this interaction may allow viral entry into the central nervous system (CNS).
Their results add to the ongoing the investigation of not only NiV pathogenesis but also to that of other important and deadly viral pathogens. The initial site of viral entry and its subsequent release and spread within a host are essential to the degree of infection and pathogenesis caused by a particular virus in its host. Spread of NiV into sub-epithelial tissues facilitates systemic infection through the host vasculature and leads to the establishment of unique sites of replication in organs systems and tissues far away from the initial portal of entry. Apical dissemination of infectious virus will also allow for host-host transmission via respiratory or urogenital epithelia.
Knowledge of how the virus achieves this spread may allow us to design better vaccines, identify novel therapeutic targets and add to the wealth of information in viral pathogenesis.
Carolin Weise, Stephanie Erbar, Boris Lamp, Carola Vogt, Sandra Diederich, and Andrea Maisner. Tyrosine Residues in the Cytoplasmic Domains Affect Sorting and Fusion Activity of the Nipah Virus Glycoproteins in Polarized Epithelial Cells. Journal of Virology, August 2010, p. 7634-7641, Vol. 84, No. 15